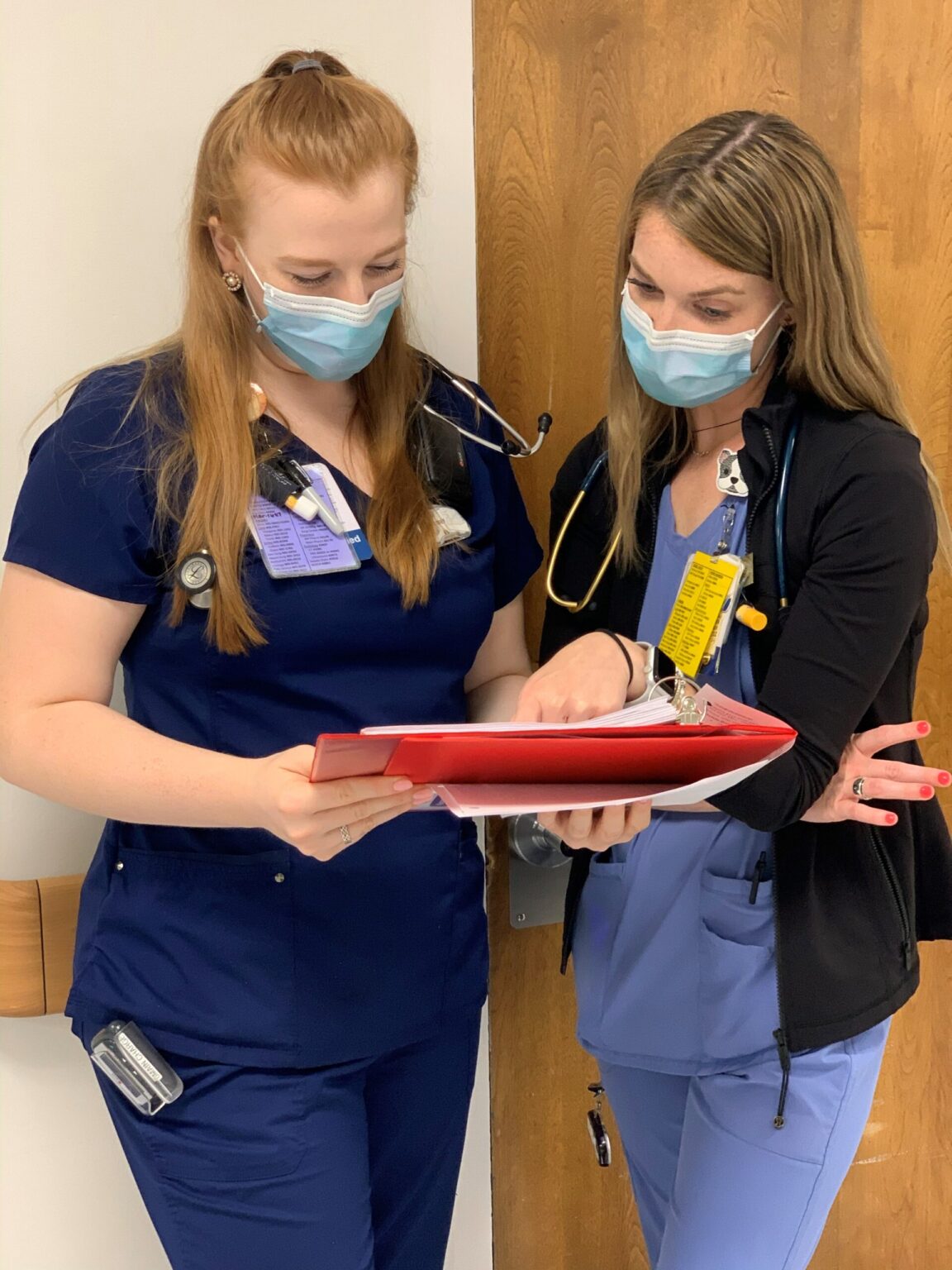
Precepting During a Pandemic
By: American Nurses Association
COVID-19’s many challenges require nurses to be even more agile and resilient. Worldwide, 162 organizations are using the Practice Transition Accreditation Program® (PTAP) framework right now to help overcome these difficult challenges.
Sarah Thornton, BSN, RN, a nurse at an academic teaching facility in Washington, DC, not only had to be resilient herself, but also teach resilience to her new graduate orientee. Sarah shared her experience with us, including how being part of a nurse residency program impacted her experience:
Preceptors are typically known as experts in an organization. If they cannot solve a problem or answer a question, they know the resources available to find the solution. However, what is to be done when one is faced with a situation in which not even the experts have the answer? That is one of the questions I recently had to ask myself. Not only was I a nurse working in one of the biggest global pandemics in recent history, I was also precepting new graduate nurses at the same time. How could I mentor them when I, myself, was not sure how to proceed? Beyond that, how could I effectively cope with the stress and mental anguish while empowering them to do the same?
Ultimately, I came to rely on the transformational leaders at my organization while looking to my peers for direct and immediate support. The teamwork, collaboration, and resultant solidarity have provided strength for us to persist. Through my words and actions, this is something that I have always modeled for new graduate nurses, though this type of behavior has become increasingly vital while precepting during the pandemic.
For example, we often touch base with a peer before entering a COVID room, so that someone is available to drop off supplies if needed. When patients begin to decline, the team engages in critical thinking. When we are having a hard time managing our emotions, we encourage resiliency amongst each other. I am fortunate to be able to say that this level of teamwork had been enculturated within my unit long before the pandemic.
I attribute this to the effective nurse residency program that my organization has implemented, as it fosters peer support from day one. This is imperative for success! When it comes down to it, we, as nurses, always need to know that we can rely on each other to provide safe care for our patients.
Sarah’s story highlights the many facets of the ANCC Practice Transition Accreditation Program® (PTAP) standards, such as peer support and teamwork, and the value they bring during even the most challenging times. These concepts are not only beneficial in a pandemic, but also provide a solid foundation for any successful transition-to-practice program. As Sarah’s story shows, accreditation ensures both preceptors and preceptees have a positive, impactful, and successful experience.
ANCC’s PTAP® accreditation features:
- A peer review process
- Integration of national competencies
- Evidence-based criteria
- Alignment with the National Academy of Medicine’s Future of Nursing recommendations
- A framework for transitioning RNs and APRNs
Discover how PTAP® accreditation can help your organization overcome challenges and establish a world-class residency program. Download your complimentary copy of the ANCC PTAP Manual and get started today!
Take the next step with our complimentary organizational self-assessment and use the gap analysis tool to help you determine how well your program aligns with the ANCC PTAP® criteria.
More suggested resources and guidance for creating and evaluating nurse residency programs are available here.


Sorry, the comment form is closed at this time.